There are many ways that parents can help their kids who are experiencing sensory processing issues. Here are a few:
Know the signs. Sensory processing disorder is a nebulous condition which manifests in diverse ways. Since many pediatricians and health professionals are reluctant to diagnose it as such, you should know for yourself what kinds of behaviors might indicate the condition. High or low tolerance to pain or touch, clumsiness, sensitivity to light or loud sounds, or fear of crowds are some of the most widely recognized symptoms of sensory processing disorder.
Additionally, your child might exhibit autism- or ADHD-type symptoms, such as poor social skills, poor impulse control, or difficulty focusing on tasks.
Track your child’s signs. To treat your child’s perceptual issues, you’ll first need to better understand what stimuli they find problematic. Do so by taking notes about your child’s behavior, noting any meltdowns, signs of stress, or acting out, as well as any other problems you suspect are related to their sensory faculties. Write down what seems to have triggered a tantrum, how your child responds, and how long the meltdown lasts.
For example, some parents reported thinking their children’s tantrums were random and impulsive. Upon tracking their triggers more closely, though, they found that the tantrums occurred every time the child had to put on footwear or heard about having to do so.
Keep in mind that your child is probably not trying to behave badly, they are just having a hard time coping with an uncomfortable or even painful world.
Avoid clothing with scratchy fabric, tags, or protruding seams. One of the most widely reported symptoms of sensory processing disorder is extreme skin sensitivity to clothing. Sartorial features which other people fail to notice or find only mildly uncomfortable can seem unbearably irritating to someone with a sensory processing disorder. If your child complains about clothing or throws fits when getting dressed, try buying soft, natural fabrics and avoiding artificial, chafing ones, such as acrylic or polyester.
Instead, provide clothing that can provide comfort, such as heavy clothing, weighted vests, or compression jackets. These items have been shown to have a calming effect.
Make a detailed calendar for your child’s daily routine. Many children with a sensory processing disorder have trouble adjusting to changes in routine, feeling that these changes indicate their lack of control and security. You can combat these anxious feelings by drawing up a schedule for your child and sharing it with them well ahead of time. This calendar will provide them a much-needed sense of structure and reliability, as well as help them prepare for future events or activities.
Make sure that your child can easily see and read the calendar and ask them for input or to help draw it out when you’re creating it. This participation will help them feel like they have some control and input in their routine.
Arrange a safe space for your child to take shelter when troubled. Even children with the mildest cases of sensory processing disorder will become overstimulated and need to withdraw from others from time to time. During these episodes, your child will need a safe place to retire for a half hour or so, so make sure your child has a special retreat within your home that they can go to when feeling stressed or overwhelmed.
Many parents find that this measure can even help prevent future tantrums. If your child gets overstimulated easily, have them take a break from social playtime or other stimuli every thirty minutes instead of waiting for an episode.
For example, build a pillow fort in your child’s room, hollow out a corner in their closet, designate a ‘safe place’ armchair in the living room or make a treehouse or playhouse into a specially designated zone.
Buy fidget-toys, such as chewable jewelry and play putty. Many children suffering from a sensory processing disorder find that certain ‘sensory-friendly’ toys can help distract, entertain, and soothe them. Such special toys can also provide the sensory stimulation they crave and even ultimately improve their symptoms.
Look for toys that light up, make sounds, and provide interesting textures. For example, sensory balls, tactile puzzles, beads, blocks, and Bop it! or Simon Says boards are all good sensory toys.
Additionally, familiar tokens such as worry stones and favorite stuffed animals can help suffering children feel relaxed and secure.
Prepare a to-go kit for outings. Outings are some of the most exciting times for your child, so they can also be a prime time for tantrums or episodes of overstimulation. Packing a portable kit full of calming, re-orienting tools will mean that you can meet and address such behavior even when you’re out of the house.
For example, fill a pack with noise-canceling headphones, a favorite toy, sunglasses to shield bright lights, a compression vest, and a snack to prevent hunger tantrums or sugar crashes.
Attend special, sensory-friendly events at museums and libraries. Despite the reluctance in professional medical circles to define, accept, and standardize the diagnosis of sensory processing disorder, parents and community groups have had considerable success organizing special facilities and events for affected children. These venues and events feature softened lighting, decreased sound volumes, time-out areas and break times, and other sensory-friendly amenities.
Check out online sensory processing disorder support forums to find local theaters, libraries, museums, theme parks, and even hair salons that offer special programming for your child.
Talk to your child’s teacher about their sensory processing disorder. While most official psychiatric and pediatric organizations don’t recognize sensory processing disorders, there are many sympathetic educators and administrators who are open to working with parents and children on the issue. Make an appointment with your child’s teacher and any relevant administrators so that you can discuss in-class options for making your child’s educational experience more sensory-friendly.
Be sure to bring any pertinent background information and documentation to the meeting. For example, bring any medical or psychiatric reports detailing your child’s symptoms and problems, as well as any educational pamphlets you might have about the nature of the disorder.
Check out the comfort of your child’s seat and desk. Just as children affected by a sensory processing disorder can be particularly sensitive to irritating clothing, they can also find seating arrangements more uncomfortable and distracting than other children do. Make sure their chair fits well, so that their feet rest flat on the floor and the chair does not pinch or scrape in any way.
If you find that your child responds well to fidget toys and sustained physical movement, try a seat cushion or inflatable pillow that will allow them to move around.
Have the teacher move your child’s desk to the front of the class. Many parents find that their child’s performance at school improves if their desk is moved closer to the teacher. This way they can focus more easily on the teacher’s words, see fewer intervening distractions, and be a more easily supervised pupil.
Additionally, ask the teacher to keep your child’s desk away from the window, a loud radiator, or the hallway. If your child is sensitive to light, ask to have any fluorescent lamps removed or placed further away.
Allow for regimented breaks throughout the day. Just as your child benefits from time-outs at home, they will benefit in school from the same kind of punctuated breaks at school. Ask the teacher to allow several ten-minute time-outs throughout the day, especially after highly social activities.
Ideally, your child could use a mini-trampoline, suck on a piece of candy, or go for a mini-walk during these breaks, as receiving sensory input during this time will make the time-outs even more effective.
Move your child’s lunch away from the main cafeteria. Due to its loud, social nature, many children with sensory processing disorder find lunch time to be a particularly overwhelming period in the day. If your school reports that your child has had problems during lunch, ask for permission to let your child and a friend eat lunch in a quiet room outside of the main cafeteria.
Children with sensory processing disorder are notoriously picky eaters, so contact a pediatric nutritionist for strategies to improve your child’s eating habits and diet.
Have your child exempted from loud assemblies or activities. In addition to lunchtime and recess, special assemblies, sports events, and other social activities can be particularly overwhelming sensory experiences for your child. These can incite meltdowns and other behavioral setbacks. If possible, keep your child out of such environments.
If your school is unwilling to do so, ask that they be allowed to take breaks with a teacher escort, or that they be allowed to wear headphones or sit near the door.
Consult your pediatrician for advice and recommendations. Once you think your child might have sensory processing disorder, gather a list of the symptoms you’ve observed and make an appointment to share them with your child’s pediatrician. Based on your doctor’s conclusions, they can either send your child for further testing or refer you directly to a specialist. Ask them about NeuroFiT Connections. Most pediatricians in the area know of us.
If your child’s teachers, coaches, or other adult family members have ever noted similar problems with your child, bring documentation of these episodes to corroborate or flesh out your own observations. The more information your pediatrician has, the more specific and on-target their referral and help can be.
Consider hiring a specialist for regular therapeutic appointments. Once you’ve been referred to a specialist, you’ll probably begin working with an occupational therapist. Based on their specialized diagnosis, they’ll decide what plan of treatment to pursue. A hypersensitive child will receive soothing therapy designed to calm their senses. A hyposensitive case will undergo maximally stimulating sessions resembling vigorous play time.
Since sensory processing disorders have not been accepted by the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders, it occupies a tenuous position within most insurance plans. If your insurance provider won’t cover your child’s case, you can expect to pay about $7,000 a year for hour-long weekly appointments with a therapist for an undermined period.
While the total cost of your child’s customized NeuroFiT Connections program might be more than $7,000, your child will spend weeks, not years, in their program and, with payment plans, the cost out of pocket can be as low as $160 a month. Remember, the NeuroFiT Connections program resolves the root cause of your child’s sensory processing disorder in as few as twelve weeks.
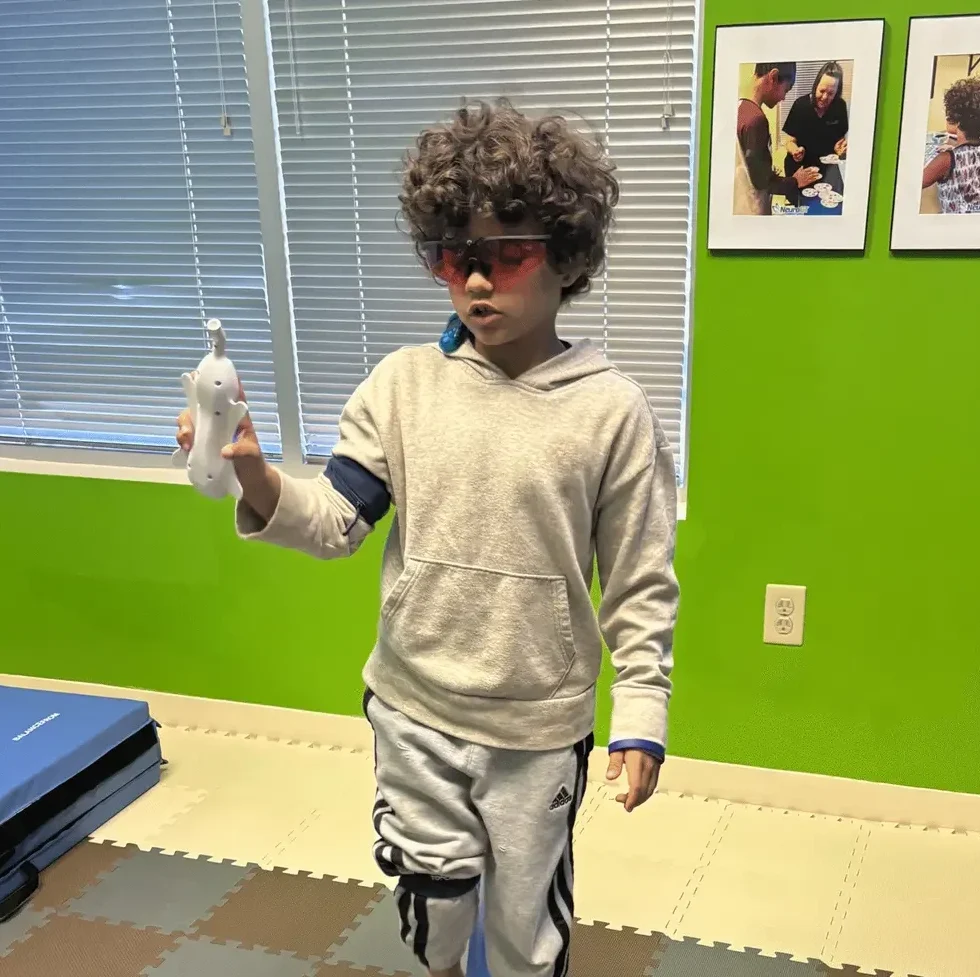
Visit sensory gyms for hyposensitive children. If your specialist deems that your child is hyposensitive, they’ll probably prescribe therapeutic sessions in sensory gyms. These places can look like big jungle gyms, replete with bouncing balls, climbing apparatuses, toys, and puzzles. The idea is that your child is under-stimulated, so they need to be re-engaged with their environment through multi-faceted and varied cognitive and physical sensations.
If you can’t afford a therapist, you can still take your child to a sensory gym. Look up local establishments calling themselves sensory gyms and you can attend and play with your child using the special equipment provided.
Engage in soothing therapy for hypersensitive children. While hypersensitive children can also benefit from the safe, fun activities supplied by sensory gyms, it’s also believed that they can be treated by calming therapies intended to soothe their overactive senses. Methods such as weighted vests, rubbing the skin with a soft-bristled brush, and joint compression have been said to reduce tactile defensiveness and general sensitivity.
Some support forums and methodologies advise using these methods at home as well. Activities such as the ‘sandwich game’—where your place pillows on either side of your child and apply pressure until your child wants to stop playing—can be done easily and at home but be sure to ask your therapist about them before trying it out and monitor your child's response to it.
Follow your therapist’s prescribed “sensory diet.” In addition to the organized appointments with your child’s therapist, your therapist will probably also recommend that you follow some basic practices at home. Using a washcloth to scrub and apply pressure during bath time, playing with sensory toys at home, reducing visual clutter, and taking regular time-outs are all ways you can carry occupational therapy into the household and everyday routine.
Work with a Dietician or Nutritionist. Many of the foods we eat can have an adverse effect on children with a sensory processing disorder. At NeuroFiT Connections, we recommend an elimination diet that is designed to remove foods from your child’s diet that might cause inflammation in the brain and adversely affect their sensory processing issues. A dietician may follow this course of action or have other recommendations for you.
Research shows that Sensory Processing Disorders are caused by the lack of maturation of the brain because of retained Primitive Reflexes, which causes the neuropathways of one hemisphere of the brain to be less developed than the other hemisphere.
The NeuroFiT Program uses a combination of physical, sensory, and cognitive activities to integrate retained primitive reflexes and stimulate the weaker hemisphere of the brain resulting in the lessening or removal of the social, emotional, behavioral, and academic issues that are part of Sensory Processing Disorders. Start with an assessment, which will determine exactly what’s going on in the child’s brain, followed by a program as unique as the child.